Friday, April 30, 2010
Rerun: Rare Footage - Me and Louis Armstrong
Following is rare archival footage of me on my didgeridoo, accompanied by Louis Armstrong. Louis, of course, is the most exciting musician to ever pick up an instrument - or sing. But here I give him a run for his money. Enjoy ...
Thursday, April 29, 2010
Charles Grassley is an Insurance Industry Shill and Enemy of the People
An article by Katherine Hobson in today’s Wall Street Journal reports that:
State chapters of the National Alliance on Mental Illness received several million dollars in contributions from pharma companies in a little less than five years, with big donations from Eli Lilly, AstraZeneca and Bristol-Myers Squibb, according to a letter from Sen. Charles Grassley.
The article cites an earlier NY Times report of NAMI national as “'hugely influential in many state capitols' for its lobbying efforts to keep states from putting any restrictions on the drugs that can be prescribed to patients covered under Medicaid and other government-funded programs."
Excuse me for breathing too loud, but it seems the only time mental illness gets any attention from the media is when someone with a mental illness shoots someone or gets shot by the police. Or when some grandstanding politician with no moral principles tries to pretend he is speaking for the people.
Anyone who has been following this blog knows I am on the board of NAMI San Diego. I have also been associated with DBSA. Both NAMI and DBSA offer free - I emphasize free, free as in free - programs and services. It has been my honor over the years to serve in the trenches alongside highly - very highly - dedicated individuals.
In a recent blog piece, I posted a video I edited of a group of soldiers serving in Iraq who organized a 5K Run in full body armor concurrent with our NAMI Walk in San Diego. Our local organization is working very hard to raise awareness for PTSD and the special needs of those who serve and have served our country.
At both DBSA and NAMI, we see - everywhere - a huge unmet need. Individuals enduring extreme personal hells. Families driven to the brink. We know what we’re talking about. Most of us serving in NAMI and DBSA have been through it. Most of us are still dealing with the challenges. Trust me, every soul I have served alongside is uncompromising in his or her belief that no one should ever - ever, ever - have to endure for one day through what they - we the people - have faced day in and day out for years and even decades on end.
Do I have to cite the terrible litany, life by life, soul by soul?
In addition, our organizations benefit from the efforts of those who have dedicated their lives to improving ours. These include enlightened clinicians and students training to enter the mental health field.
Alas, a huge unmet need. Alas, precious few resources. One drop of commitment into a vast bottomless black hole of suffering.
Sad to say, mental illness lacks the cachet of the glamor diseases. High society does not write out six figure checks to support our cause. Hollywood doesn’t rally behind us. Politicians look the other way.
We look around, we in the trenches. We see vital services cut. We see people cut off, cut out. We field their calls for help. We’re there when they walk through the door. But there is only so much we can do. We roll up our sleeves and do what we can. Then we scrap, we hustle, we lift the seat cushions for whatever loose change happens to roll to the floor.
I’m not going to lower myself by responding to Grassley’s shameless accusations and innuendos. But I will note this:
According to OpenSecrets.org, Sen Grassley received $279,118 in campaign contributions from the insurance industry from 2005 to 2010. He voted against health care reform.
The Senator from Iowa is part of the problem, not the solution. He needs to be called out for the paid industry shill and an enemy of the people he truly is.
Thanks. I needed that. Time for me to breathe a little less loudly. Thank you for your patience.
Disclosure: I am on the board of NAMI San Diego. What I said here is my own opinion entirely and does not represent NAMI San Diego or any individuals or organizations it is affiliated with.
State chapters of the National Alliance on Mental Illness received several million dollars in contributions from pharma companies in a little less than five years, with big donations from Eli Lilly, AstraZeneca and Bristol-Myers Squibb, according to a letter from Sen. Charles Grassley.
The article cites an earlier NY Times report of NAMI national as “'hugely influential in many state capitols' for its lobbying efforts to keep states from putting any restrictions on the drugs that can be prescribed to patients covered under Medicaid and other government-funded programs."
Excuse me for breathing too loud, but it seems the only time mental illness gets any attention from the media is when someone with a mental illness shoots someone or gets shot by the police. Or when some grandstanding politician with no moral principles tries to pretend he is speaking for the people.
Anyone who has been following this blog knows I am on the board of NAMI San Diego. I have also been associated with DBSA. Both NAMI and DBSA offer free - I emphasize free, free as in free - programs and services. It has been my honor over the years to serve in the trenches alongside highly - very highly - dedicated individuals.
In a recent blog piece, I posted a video I edited of a group of soldiers serving in Iraq who organized a 5K Run in full body armor concurrent with our NAMI Walk in San Diego. Our local organization is working very hard to raise awareness for PTSD and the special needs of those who serve and have served our country.
At both DBSA and NAMI, we see - everywhere - a huge unmet need. Individuals enduring extreme personal hells. Families driven to the brink. We know what we’re talking about. Most of us serving in NAMI and DBSA have been through it. Most of us are still dealing with the challenges. Trust me, every soul I have served alongside is uncompromising in his or her belief that no one should ever - ever, ever - have to endure for one day through what they - we the people - have faced day in and day out for years and even decades on end.
Do I have to cite the terrible litany, life by life, soul by soul?
In addition, our organizations benefit from the efforts of those who have dedicated their lives to improving ours. These include enlightened clinicians and students training to enter the mental health field.
Alas, a huge unmet need. Alas, precious few resources. One drop of commitment into a vast bottomless black hole of suffering.
Sad to say, mental illness lacks the cachet of the glamor diseases. High society does not write out six figure checks to support our cause. Hollywood doesn’t rally behind us. Politicians look the other way.
We look around, we in the trenches. We see vital services cut. We see people cut off, cut out. We field their calls for help. We’re there when they walk through the door. But there is only so much we can do. We roll up our sleeves and do what we can. Then we scrap, we hustle, we lift the seat cushions for whatever loose change happens to roll to the floor.
I’m not going to lower myself by responding to Grassley’s shameless accusations and innuendos. But I will note this:
According to OpenSecrets.org, Sen Grassley received $279,118 in campaign contributions from the insurance industry from 2005 to 2010. He voted against health care reform.
The Senator from Iowa is part of the problem, not the solution. He needs to be called out for the paid industry shill and an enemy of the people he truly is.
Thanks. I needed that. Time for me to breathe a little less loudly. Thank you for your patience.
Disclosure: I am on the board of NAMI San Diego. What I said here is my own opinion entirely and does not represent NAMI San Diego or any individuals or organizations it is affiliated with.
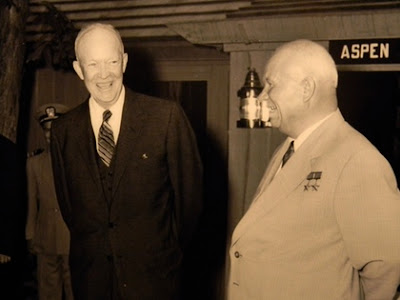
More on Eisenhower

Eisenhower was a unifier, a consensus-builder. A Republican, he viewed Democrats as collaborators rather than political enemies. This was a skill he acquired as Supreme Commander of the allied armies during World War II, where dealing with the likes of de Gaulle and Montgomery often proved far more problematic than fighting Rommel’s Germans.
Fortunately, Ike served in an era of consensus-builders - political statesmen who put the public good above their own partisan interests. In today's political and media climate, he might have trouble finding a single political partner to collaborate with. Instead, with a little help from his friends (including Democratic Senate Majority Leader LBJ), he presided over a decade that people now look back upon (often erroneously) with a sense of nostalgia.
Last week, while in Kansas to keynote the state DBSA conference, I paid a visit to the Eisenhower Presidential Library and Museum in Abilene.
The home Ike grew up in.
General Eisenhower inspecting a liberated Nazi death camp. Significantly, as one all too familiar with the realities and limitations of war, one of his first accomplishments as President was to end the bloody stalemate in Korea. Throughout his Administration, he proved exceptionally adept at waging peace.
Nevertheless, Ike aggressively faced down the Soviet challenge. This was an age of comical air raid drills, but the stakes were deadly earnest. Thanks in large part to Ike, the Cold War remained cold.
My answer to anyone who spouts mindless nonsense about big government: "How was your drive here?"
Ike was the prime mover for the Interstate Highway System that we all take for granted, that none of us can do without. Brought to you by big government. Also, thanks to Ike and big government: The space program, expanded social security, and a strong military deterrence.
"Ike was with us when America needed him." - LBJ.
See also: An Eisenhower Appreciation
Wednesday, April 28, 2010
NAMI Runs in Iraq
You have to watch this.
On April 17, concurrent with the NAMI San Diego Walk for mental health awareness taking place in Balboa Park, John Bell and members of his Army unit in Iraq ran 5K in full body armor. One in six veterans of Iraq and Afghanistan is affected by PTSD, depression, or anxiety. Only half seek help.
Tuesday, April 27, 2010
An Eisenhower Appreciation

When I visited Kansas last week to keynote the DBSA State Conference in Manhattan, I made a side trip to Abilene, where Dwight Eisenhower grew up and where the Eisenhower Presidential Museum and Library is located.
I’ve long argued that Eisenhower is a very underrated President. Coming after Roosevelt and Truman, it is easy to see why. But now that we have ten Presidents who came later to compare him to, there is no question as to his rightful place in history.
As a military commander who sent men into battle, Eisenhower knew all too well the realities of war and its limitations. Significantly, he began his Presidency by ending a war (in Korea). Throughout his Presidency, he proved astonishingly adept at keeping the peace, while at the same time successfully containing the Soviet threat. The quotes below provide an excellent insight into the mind of the man:
More later ...
Sunday, April 25, 2010
Rerun: ANZAC Day - Quiet Remembrance
.jpg)
This from last year ...
It was supposed to be a quick and easy campaign. But British military incompetence blew the element of surprise. On April 25, 1915, British allied forces - including a large contingent of Australian and New Zealand units (ANZACs) - landed on the beaches of the Gallipoli Peninsula in Turkey only to encounter waiting Turkish forces dug in on the heights.
The intention had been to quickly knock Turkey out of the war (World War I), thereby rendering Germany vulnerable to invasion from the south. Instead, the allies found themselves on the defensive, clinging to the small bits of land they had gained in the early days of fighting. In one desperate battle, 17,000 ANZACs held off 42,000 Turks.
Several months into the campaign, ANZAC troops spearheaded an offensive to seize the high ground. New Zealand's Wellington Brigade managed to fight its way to the summit of Chunuk Bair, only to be swept off the top by a force led in person by Mustafa Kemal, who would later become known as Ataturk, founder of modern Turkey. Of the 760 ANZACs who made it to the top, 711 became casualties.
The campaign ground down into brutal trench warfare. The troops, exposed to the heat and appallingly unsanitary conditions, were mowed down this time by dysentery. By the end of summer it became apparent that the campaign was a failure, but it took until early January 1916 to organize and complete an evacuation.
More than 10,000 ANZACs lost their lives during the Gallipoli campaign, which ushered in a coming of age for both nations. In the wake of that senseless bloodbath in distant Turkey, men and women in a far-flung corner of the British Empire came to regard themselves as Australians and New Zealanders rather than mere British subjects.
ANZACs also saw service as cannon fodder on the European front, where they suffered more casualties per population than the other forces in the war.
It is dawn in New Zealand right now, one day ahead of the US. New Zealanders of all ages right now are gathered at the war memorials that grace every town there, large and small. Simply counting the names of the dead inscribed into those memorials is a sobering exercise. The ceremony is simple and solemn.
I lived in New Zealand for 11 years, Australia for 5. As well as my US citizenship, I also hold New Zealand citizenship. My daughter was born and raised in New Zealand. She resides in Wellington with her husband, another New Zealander. Any children they may have will be New Zealanders.
The sun is rising in New Zealand right now. A bugler is about to sound Last Post. It is time for two minutes of silence, a quiet remembrance.
Postscript: I'm proud to say I now have a grandson - Teddy, seven months - a New Zealander.
Friday, April 23, 2010
iPhone Photo of the Day: Little House on the Prairie
I shot this yesterday, just outside Manhattan, Kansas. Today, a new Kansas buddy and I drove 40 miles to Abilene to visit the Eisenhower Library and Museum (much more in a future blog). Tomorrow I'm keynoting the DBSA Kansas State Conference. I'm back in my hotel, where I spent the evening going over the two talks I will be presenting.
Big day tomorrow. To bed ...
Big day tomorrow. To bed ...
Labels:
iPhone,
John McManamy,
Kansas DBSA,
photo of the day
Thursday, April 22, 2010
iPhone Photo of the Day: Prairie Sky
This was shot this afternoon from the passenger seat headed west toward Manhattan, Kansas. I'll be keynoting the DBSA Kansas State Conference on Saturday.
Labels:
iPhone,
John McManamy,
Kansas DBSA,
photo of the day
Wednesday, April 21, 2010
Back When Psychiatry Was (Sort of) Enlightened
I'm in a downtown hotel right now, ready to fly out to Kansas tomorrow to give two talks as the keynoter at the Kansas State DBSA conference, to take place Saturday in Manhattan. Following is a segment from my second talk ...
My research often takes me to strange places. This little adventure started in front of my computer. One day, for the heck of it, I checked out the very first issue of the American Journal of Psychiatry, which came out in 1844. Back then it was called The American Journal of Insanity.
The American Journal of Psychiatry is published by the American Psychiatric Association, which was also founded in 1844.
Now, you heard me mention this morning how modern brain science is showing that stress makes us sitting ducks for all kinds of mental illness and other weird stuff. And I also mentioned that psychiatry already knew this back in 1952 when the first DSM came out. As it turns out, the principle was already an old one back in 1844.
Of all things, this first issue of the Journal of Insanity had a long article dealing with Shakespeare. Cool, I thought. So I started reading. This from King Lear:
Be comforted, good Madam, the great rage You see is cured in him, and yet it is danger To make him even o’er the time he has lost; Desire him to go in, trouble him no more Till further settling.
As the Journal observed:
Now we confess, almost with shame, that although near two centuries and a half have passed since Shakespeare thus wrote; we have very little to add to his method of treating the insane.
Wow. So this is an ancient principle, then. And the modern psychiatric science of 1844 just validated it.
The Journal goes on to say:
To produce sleep and to quiet the mind by medical and moral treatment, to avoid all unkindness, and when patients begin to convalesce, to guard, as he directs, against everything likely to disturb their minds, and to cause a relapse is now considered the best and nearly the only essential treatment.
Hold on a sec ... Wasn’t 1844 supposed to be the Dark Ages? Weren’t asylums terrible places where they locked away - “the insane”?
Well, it turns out the 1830s and 40s was a great reform era. Abraham Lincoln came of age around this time. This was a time of enlightened science meeting enlightened Christianity. Have you had a look at the buildings and grounds of these old institutions? They were beautiful. Palatial country estates.
They even had farms attached to them.
Well, talk about coincidence. It turns out that this same 1844 Journal - the one that had a long piece on Shakespeare - also had a report describing an institution in Utica, then in operation for 18 months. According to the report, of 433 patients admitted, 123 had recovered.
Okay - we can’t be sure what the report meant by the term, recovery. But it is fair to assume that in an age of no psychiatric meds or other treatments - or so-called “treatments” that made patients worse - more than one-quarter of those admitted were deemed to be in good enough condition to return to their homes and communities.
About a year after I came across that 1844 psychiatry journal, I found myself in LA. I was on my way to my daughter’s wedding in New Zealand and I was staying at a friend’s house before flying out.
I don’t know about you, but I don’t look forward to holidays. Because that means I have to crank out three weeks worth of work in just one week. So here I am, in LA, all worked out - stressed, if you like, needing to relax, needing to get away from work.
I should have known. Maybe a lot of you know this already. If you’re a mental health advocate, you really gotta watch hanging out with fellow mental health advocates. So what’s my friend’s idea of a good night on the town? Attending a three-hour lecture on mental health, that’s what.
Great. I’m in vacation mode. I want to forget about work, and here I am being dragged out into the night to sit in on a university class for some psychology majors at USC. A leading world authority on psychiatric rehabilitation, Robert Liberman of UCLA is giving a guest lecture.
Well, I decide to go with my friend, but that doesn’t mean I have to listen. Anyway, here I am, in a college classroom, trying very hard not to listen, when suddenly Dr Liberman starts telling us how the insane asylums of old were very enlightened places, with high recovery rates.
My ears pricked up. Wait? Hadn't I read something like this?
Dr Liberman went on to say in so many words that mental illness was a product of the industrial age. Jam people into cities and watch what happens.
Asylums were built to get people away from all that. Only later, he explained, did cash-strapped state governments give up on us.
Of all things, on the ride back, I’m thanking my friend profusely for dragging me out into the night.
Catch me in Kansas. For further details ...
My research often takes me to strange places. This little adventure started in front of my computer. One day, for the heck of it, I checked out the very first issue of the American Journal of Psychiatry, which came out in 1844. Back then it was called The American Journal of Insanity.
The American Journal of Psychiatry is published by the American Psychiatric Association, which was also founded in 1844.
Now, you heard me mention this morning how modern brain science is showing that stress makes us sitting ducks for all kinds of mental illness and other weird stuff. And I also mentioned that psychiatry already knew this back in 1952 when the first DSM came out. As it turns out, the principle was already an old one back in 1844.
Of all things, this first issue of the Journal of Insanity had a long article dealing with Shakespeare. Cool, I thought. So I started reading. This from King Lear:
Be comforted, good Madam, the great rage You see is cured in him, and yet it is danger To make him even o’er the time he has lost; Desire him to go in, trouble him no more Till further settling.
As the Journal observed:
Now we confess, almost with shame, that although near two centuries and a half have passed since Shakespeare thus wrote; we have very little to add to his method of treating the insane.
Wow. So this is an ancient principle, then. And the modern psychiatric science of 1844 just validated it.
The Journal goes on to say:
To produce sleep and to quiet the mind by medical and moral treatment, to avoid all unkindness, and when patients begin to convalesce, to guard, as he directs, against everything likely to disturb their minds, and to cause a relapse is now considered the best and nearly the only essential treatment.
Hold on a sec ... Wasn’t 1844 supposed to be the Dark Ages? Weren’t asylums terrible places where they locked away - “the insane”?
Well, it turns out the 1830s and 40s was a great reform era. Abraham Lincoln came of age around this time. This was a time of enlightened science meeting enlightened Christianity. Have you had a look at the buildings and grounds of these old institutions? They were beautiful. Palatial country estates.
They even had farms attached to them.
Well, talk about coincidence. It turns out that this same 1844 Journal - the one that had a long piece on Shakespeare - also had a report describing an institution in Utica, then in operation for 18 months. According to the report, of 433 patients admitted, 123 had recovered.
Okay - we can’t be sure what the report meant by the term, recovery. But it is fair to assume that in an age of no psychiatric meds or other treatments - or so-called “treatments” that made patients worse - more than one-quarter of those admitted were deemed to be in good enough condition to return to their homes and communities.
About a year after I came across that 1844 psychiatry journal, I found myself in LA. I was on my way to my daughter’s wedding in New Zealand and I was staying at a friend’s house before flying out.
I don’t know about you, but I don’t look forward to holidays. Because that means I have to crank out three weeks worth of work in just one week. So here I am, in LA, all worked out - stressed, if you like, needing to relax, needing to get away from work.
I should have known. Maybe a lot of you know this already. If you’re a mental health advocate, you really gotta watch hanging out with fellow mental health advocates. So what’s my friend’s idea of a good night on the town? Attending a three-hour lecture on mental health, that’s what.
Great. I’m in vacation mode. I want to forget about work, and here I am being dragged out into the night to sit in on a university class for some psychology majors at USC. A leading world authority on psychiatric rehabilitation, Robert Liberman of UCLA is giving a guest lecture.
Well, I decide to go with my friend, but that doesn’t mean I have to listen. Anyway, here I am, in a college classroom, trying very hard not to listen, when suddenly Dr Liberman starts telling us how the insane asylums of old were very enlightened places, with high recovery rates.
My ears pricked up. Wait? Hadn't I read something like this?
Dr Liberman went on to say in so many words that mental illness was a product of the industrial age. Jam people into cities and watch what happens.
Asylums were built to get people away from all that. Only later, he explained, did cash-strapped state governments give up on us.
Of all things, on the ride back, I’m thanking my friend profusely for dragging me out into the night.
Catch me in Kansas. For further details ...
Tuesday, April 20, 2010
The DSM-5: Science vs Scientism
Just a quick note before I start packing for Kansas. Nassir Ghaemi MD of Tufts (pictured here), who has helped me enormously in understanding the fine points of my illness over the years, has cited one of my blogs pieces here with approval.
In a blog post on Medscape, Dr Ghaemi neatly encapsulates the DSM-5 debate. To quote at length:
In recent months, there has been back-and-forth between the heads of DSM-III (Robert Spitzer) and DSM-IV (Allen Frances), on one side, and the leaders of DSM-V (David Kupfer and colleagues), on the other. Frances in particular has been vocal in articles in the Psychiatric Times and the British Journal of Psychiatry; his critique sums up this way:
Changes in DSM-V should not be made unless strong scientific evidence exists to do so. A conservative baseline mind-set appears to exist such that revisions should always err on the side of not making a change unless notably strong evidence exists for change. The rationale, as Frances describes it, is partly so that the psychiatric profession is protected from rapid and unnecessary changes in nosology.
Dr. Frances does not seem to question the validity of his assumptions: Should we have a very high threshold for making changes? Should we be erring on the side of not making changes?
As John McManamy notes, this would ensure that we would forever be mired in the "Groundhog Day of 1980", the last time anyone in psychiatry had the courage to structurally change our nosology.
Science, yes; scientism, no. We should not let claims of science blind us to data that are good enough, or to current practice that has the virtue of not requiring change but the vice of being unscientific.
As I noted in other pieces here, the DSM-5 is not a science project. Instead of an academic publication that maybe 30 people would read, the DSM is a real world document relied upon by millions. Ironically, in the name of science, the DSM-5 is leaving in place ancient diagnostic criteria the defies both science and reality (such as not acknowledging the depression-bipolar spectrum).
As Dr Ghaemi concludes:
Over time, revolutionaries tend to become conservatives, and reaction engenders counter-reaction. There is a psychological law of inertia, as the writer Henry Adams observed: What exists is valued simply because it exists, and much more effort is needed to push the boulder of dogma into motion than to leave it alone. Perhaps the physicist Max Planck is sadly all too right that new scientific truths are routinely resisted by prior generations, who are rarely convinced, and rather are only accepted by a changing of generations.
In a blog post on Medscape, Dr Ghaemi neatly encapsulates the DSM-5 debate. To quote at length:
In recent months, there has been back-and-forth between the heads of DSM-III (Robert Spitzer) and DSM-IV (Allen Frances), on one side, and the leaders of DSM-V (David Kupfer and colleagues), on the other. Frances in particular has been vocal in articles in the Psychiatric Times and the British Journal of Psychiatry; his critique sums up this way:
Changes in DSM-V should not be made unless strong scientific evidence exists to do so. A conservative baseline mind-set appears to exist such that revisions should always err on the side of not making a change unless notably strong evidence exists for change. The rationale, as Frances describes it, is partly so that the psychiatric profession is protected from rapid and unnecessary changes in nosology.
Dr. Frances does not seem to question the validity of his assumptions: Should we have a very high threshold for making changes? Should we be erring on the side of not making changes?
As John McManamy notes, this would ensure that we would forever be mired in the "Groundhog Day of 1980", the last time anyone in psychiatry had the courage to structurally change our nosology.
Science, yes; scientism, no. We should not let claims of science blind us to data that are good enough, or to current practice that has the virtue of not requiring change but the vice of being unscientific.
As I noted in other pieces here, the DSM-5 is not a science project. Instead of an academic publication that maybe 30 people would read, the DSM is a real world document relied upon by millions. Ironically, in the name of science, the DSM-5 is leaving in place ancient diagnostic criteria the defies both science and reality (such as not acknowledging the depression-bipolar spectrum).
As Dr Ghaemi concludes:
Over time, revolutionaries tend to become conservatives, and reaction engenders counter-reaction. There is a psychological law of inertia, as the writer Henry Adams observed: What exists is valued simply because it exists, and much more effort is needed to push the boulder of dogma into motion than to leave it alone. Perhaps the physicist Max Planck is sadly all too right that new scientific truths are routinely resisted by prior generations, who are rarely convinced, and rather are only accepted by a changing of generations.
Labels:
draft DSM-5,
draft DSM-V,
John McManamy,
Nassir Ghaemi
Mindfulness - The Ultimate Mood Stabilizer
I'm preparing a keynote I will be presenting to the Kansas DBSA State Conference on Saturday (see side panel for details). Part of my talk will focus on mindfulness, which meant going back over some of my earlier pieces on the topic. Following is an extract from a longer piece on mcmanweb. Enjoy:
“Mind precedes its objects,” reads the first line of the Dhammapada, the best-known of the Buddhist scriptures. “They are mind-governed and mind-made. To speak or act with a defiled mind is to draw pain after oneself, like a wheel behind the feet of the animal drawing it.”
Further down, we read: “A disciplined mind leads to happiness.”
Jon Kabat-Zinn PhD of the University of Massachusetts is a molecular biologist and meditation teacher. In his new book (with three co-authors), “The Mindful Way Through Depression,” Dr Kabat-Zinn urges cultivating awareness by not taking our thoughts so literally and by “disengaging the autopilot.”
Mindfulness, say the authors, “is the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to things as they are,” rather than as we want them to be.
If I felt myself becoming unduly agitated, I would typically take a “time-out” from my routine. If I felt myself starting to feel sorry for myself or getting depressed, I would make it a point to get out of the house. On and on it went, all the little coping tricks. Things we do all the time.
Half the trick of mindfulness is being able to spot your mood episodes as they begin - or even before they begin - while you are still in control of your brain, while you still have choices. Most of the time, the solution is fairly simple - a time-out, a break, some quiet moments, a good night’s sleep.
The other half of mindfulness is detachment. Detachment is a key part of Buddhist teaching. When the mind watches the mind, the skillful person does so with practiced disinterest, as if observing the grass growing or the paint drying. Mind you, detachment is way easier said than done, especially when you sense your brain is on the process of rapid disintegration.
Mindfulness begins with the painful reminder that life is not safe. We are vulnerable. Nothing is fixed. Our situation is constantly changing around us. Psychologically speaking, we are always walking at midnight in a bad neighborhood. We need to be awake. We need to be vigilant.
But we have a paradox at play, here. As we grow more adept at mindfulness techniques, our lives become more safe, our existence less fearful. Hypomania no longer has to automatically mean a prelude to mania. And a bad hair day is not necessarily the end of the world.
Bipolar has been called “a dangerous gift,” one that many of us would gladly return to the customer service counter of life. The practice of mindfulness opens up the possibility of realizing our potential, but it also necessitates working within our limitations and leading highly disciplined lives. It means calling it a night when the party is just getting started. It means chilling out in the middle of a productive hot streak. It means maintaining our composure when we feel our situation or our lives falling apart.
We all employ mindfulness to some degree, but cultivating the practice is going to take time. Mindfulness is no quick fix. It is advisable to stay on your current meds doses until you have your high dose mindfulness and other recovery practices well in place. Even then, knowing when to bump your meds doses back up should be part of your mindfulness game plan.
Be mindful. Live well ...
Also check out:
Mindfulness - Living in the Present
“Mind precedes its objects,” reads the first line of the Dhammapada, the best-known of the Buddhist scriptures. “They are mind-governed and mind-made. To speak or act with a defiled mind is to draw pain after oneself, like a wheel behind the feet of the animal drawing it.”
Further down, we read: “A disciplined mind leads to happiness.”
Jon Kabat-Zinn PhD of the University of Massachusetts is a molecular biologist and meditation teacher. In his new book (with three co-authors), “The Mindful Way Through Depression,” Dr Kabat-Zinn urges cultivating awareness by not taking our thoughts so literally and by “disengaging the autopilot.”
Mindfulness, say the authors, “is the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to things as they are,” rather than as we want them to be.
If I felt myself becoming unduly agitated, I would typically take a “time-out” from my routine. If I felt myself starting to feel sorry for myself or getting depressed, I would make it a point to get out of the house. On and on it went, all the little coping tricks. Things we do all the time.
Half the trick of mindfulness is being able to spot your mood episodes as they begin - or even before they begin - while you are still in control of your brain, while you still have choices. Most of the time, the solution is fairly simple - a time-out, a break, some quiet moments, a good night’s sleep.
The other half of mindfulness is detachment. Detachment is a key part of Buddhist teaching. When the mind watches the mind, the skillful person does so with practiced disinterest, as if observing the grass growing or the paint drying. Mind you, detachment is way easier said than done, especially when you sense your brain is on the process of rapid disintegration.
Mindfulness begins with the painful reminder that life is not safe. We are vulnerable. Nothing is fixed. Our situation is constantly changing around us. Psychologically speaking, we are always walking at midnight in a bad neighborhood. We need to be awake. We need to be vigilant.
But we have a paradox at play, here. As we grow more adept at mindfulness techniques, our lives become more safe, our existence less fearful. Hypomania no longer has to automatically mean a prelude to mania. And a bad hair day is not necessarily the end of the world.
Bipolar has been called “a dangerous gift,” one that many of us would gladly return to the customer service counter of life. The practice of mindfulness opens up the possibility of realizing our potential, but it also necessitates working within our limitations and leading highly disciplined lives. It means calling it a night when the party is just getting started. It means chilling out in the middle of a productive hot streak. It means maintaining our composure when we feel our situation or our lives falling apart.
We all employ mindfulness to some degree, but cultivating the practice is going to take time. Mindfulness is no quick fix. It is advisable to stay on your current meds doses until you have your high dose mindfulness and other recovery practices well in place. Even then, knowing when to bump your meds doses back up should be part of your mindfulness game plan.
Be mindful. Live well ...
Also check out:
Mindfulness - Living in the Present
Sunday, April 18, 2010
My NAMI San Diego Walk Video
Enjoy ...
(This is the high def version that replaces my low def version I had uploaded earlier.)
Scenes From the NAMI San Diego Walk
Balboa Park, Saturday, way too early in the morning.
Walk organizer, Annie.
NAMI doer-of-everything, Rita. She is pictured here, reacting to a rumor that didgeridoos have been banned from NAMI walks.
Little does Rita know ... I'm handing out didgeridoos to kids like candy. More to come ...
Walk organizer, Annie.
NAMI doer-of-everything, Rita. She is pictured here, reacting to a rumor that didgeridoos have been banned from NAMI walks.
Little does Rita know ... I'm handing out didgeridoos to kids like candy. More to come ...
Friday, April 16, 2010
I Walk So That Others May Cheat in Scrabble
I have no idea what that means.
Tomorrow, I walk for NAMI San Diego. I cordially invite those of you living within jumbo jet distance of San Diego to join me tomorrow. Watch out for the volcanic dust.
I also invite all of you to support me in my walk by making an online donation.
I know a lot of you like to wait till the last minute to donate. This is the last minute.
I serve on the board of NAMI San Diego, and I devote a lot of time to the organization. We are leaders in making vital outreaches to the community, but we need your help.
If you like what I do on this blog, this is your way of showing your appreciation. Many thanks to those of you who have already shown their support.
Tomorrow, I walk for NAMI San Diego. I cordially invite those of you living within jumbo jet distance of San Diego to join me tomorrow. Watch out for the volcanic dust.
I also invite all of you to support me in my walk by making an online donation.
I know a lot of you like to wait till the last minute to donate. This is the last minute.
I serve on the board of NAMI San Diego, and I devote a lot of time to the organization. We are leaders in making vital outreaches to the community, but we need your help.
If you like what I do on this blog, this is your way of showing your appreciation. Many thanks to those of you who have already shown their support.
Craig Venter: Hypomanic
Following is an extract from a lengthy review I first published in my Newsletter in late 2004, and on mcmanweb in 2005 ...
"Up until 2003, only God could claim to have created life. The Almighty must now share that honor with a hypomanic American."
That provocative statement comes from the book, "The Hypomanic Edge: The Link Between (a Little) Craziness and (a Lot of) Success in America" by John Gartner PhD.
Dr Gartner is an associate professor of psychiatry at Johns Hopkins. The book invites an obvious comparison to one published in 2004 by his university colleague Kay Jamison PhD, "Exuberance: The Passion for Life". But that book downplayed the bipolar connection, much to the disappointment of many admirers of her previous "Touched with Fire."
Not so with Dr Gartner’s work, which contends that America would not be what it is today without the hypomanic drive of the people who settled, founded, and shaped a nation in their image. Exhibit A is God’s partner in creating life, Craig Venter.
Readers may recall a June 2000 White House ceremony in which President Clinton announced a "tie" between two competing groups to sequence the human genome: the official government effort, the Human Genome Project (HGP) headed up by Francis Collins and a breakaway private venture bankrolled by a new company, Celera, run by maverick geneticist Craig Venter.
In fact, the tie was a political sham engineered by the White House with the collusion of both parties. Celera had actually run rings around the opposition, smoked them, waxed them, wiped the floor with their face. It wasn’t even close. Not only had Celera crossed the finish line well ahead of the HGP, it delivered a more complete genetic blueprint. To add insult to injury, the only way the HGP could even stay in the race was by scrapping its own plodding methods and game plan for Celera’s.
Craig Venter was a wild man from day one. As a kid, he liked to race his bike on the local airport runway as planes took off. In the Army, he frequently got on the wrong side of his superiors. On acceptance to a university faculty position, he wasted no time turning colleagues into enemies, then evinced surprise when they refused to grant him tenure. He arrived at the NIH and caught the attention of his hero, James Watson, but became disillusioned when the great man tactlessly treated him as a mere technician and publicly humiliated him in a Senate hearing.
Venter acknowledged to Dr Gartner that he probably has "a very mild case of manic depression." When the author described bipolar II to him, he replied, "That characterizes some pretty big stretches of my life."
Driven into the private sector, Venter in 1995 revolutionized microbiology by successfully mapping the H flu genome using a novel "shotgun" method. At the time, the HGP was in full swing. Three years later, with the support of Celera, Venter made the surprise announcement that he would map the human genome four years ahead of the HGP’s target date at one tenth the cost. As Dr Gartner describes it: "What psychiatrists call ‘impulsivity,’ entrepreneurs call ‘seizing the moment.’"
Venter added that Collins’ team should just quit now and stick to mapping the mouse.
A few days later he turned up uninvited at a HGP meeting and taunted the participants. One scientist wanted to slug him and another strangle him. But the affront energized the opposition and instilled in them a newfound sense of urgency. Meanwhile, Venter mobilized his troops with the charismatic élan of a battlefield commander. A colleague compared his efforts to high dives into empty pools, timed so that the water would be there by the time he hit bottom.
In the end, Venter nailed all his landings, a full five years ahead of HGP’s original schedule. Under the terms of the White House agreement, neither party was supposed to attack the other’s work, but embittered HGP scientists simply couldn’t help themselves. Even Mother Teresa would hate the guy.
Venter proved equally successful in alienating his financial backers. In 2002, Celera fired him and he went into a depression, only to bounce back as head of the privately-funded "Genesis Project," which effectively created life by building a virus from scratch. A team at the State University of New York at Stony Book had accomplished a similar feat shortly before, but their effort had taken three years compared to Venter’s 14 days.
Now science was truly playing God, for better or for worse, with the potential to transform the world or destroy it. It’s the kind of challenge that hypomanics live for.
See the full review on mcmanweb
Columbus, religious dissidents, Alexander Hamilton, Andrew Carnegie, the Hollywood moguls ...
"Up until 2003, only God could claim to have created life. The Almighty must now share that honor with a hypomanic American."
That provocative statement comes from the book, "The Hypomanic Edge: The Link Between (a Little) Craziness and (a Lot of) Success in America" by John Gartner PhD.
Dr Gartner is an associate professor of psychiatry at Johns Hopkins. The book invites an obvious comparison to one published in 2004 by his university colleague Kay Jamison PhD, "Exuberance: The Passion for Life". But that book downplayed the bipolar connection, much to the disappointment of many admirers of her previous "Touched with Fire."
Not so with Dr Gartner’s work, which contends that America would not be what it is today without the hypomanic drive of the people who settled, founded, and shaped a nation in their image. Exhibit A is God’s partner in creating life, Craig Venter.
Readers may recall a June 2000 White House ceremony in which President Clinton announced a "tie" between two competing groups to sequence the human genome: the official government effort, the Human Genome Project (HGP) headed up by Francis Collins and a breakaway private venture bankrolled by a new company, Celera, run by maverick geneticist Craig Venter.
In fact, the tie was a political sham engineered by the White House with the collusion of both parties. Celera had actually run rings around the opposition, smoked them, waxed them, wiped the floor with their face. It wasn’t even close. Not only had Celera crossed the finish line well ahead of the HGP, it delivered a more complete genetic blueprint. To add insult to injury, the only way the HGP could even stay in the race was by scrapping its own plodding methods and game plan for Celera’s.
Craig Venter was a wild man from day one. As a kid, he liked to race his bike on the local airport runway as planes took off. In the Army, he frequently got on the wrong side of his superiors. On acceptance to a university faculty position, he wasted no time turning colleagues into enemies, then evinced surprise when they refused to grant him tenure. He arrived at the NIH and caught the attention of his hero, James Watson, but became disillusioned when the great man tactlessly treated him as a mere technician and publicly humiliated him in a Senate hearing.
Venter acknowledged to Dr Gartner that he probably has "a very mild case of manic depression." When the author described bipolar II to him, he replied, "That characterizes some pretty big stretches of my life."
Driven into the private sector, Venter in 1995 revolutionized microbiology by successfully mapping the H flu genome using a novel "shotgun" method. At the time, the HGP was in full swing. Three years later, with the support of Celera, Venter made the surprise announcement that he would map the human genome four years ahead of the HGP’s target date at one tenth the cost. As Dr Gartner describes it: "What psychiatrists call ‘impulsivity,’ entrepreneurs call ‘seizing the moment.’"
Venter added that Collins’ team should just quit now and stick to mapping the mouse.
A few days later he turned up uninvited at a HGP meeting and taunted the participants. One scientist wanted to slug him and another strangle him. But the affront energized the opposition and instilled in them a newfound sense of urgency. Meanwhile, Venter mobilized his troops with the charismatic élan of a battlefield commander. A colleague compared his efforts to high dives into empty pools, timed so that the water would be there by the time he hit bottom.
In the end, Venter nailed all his landings, a full five years ahead of HGP’s original schedule. Under the terms of the White House agreement, neither party was supposed to attack the other’s work, but embittered HGP scientists simply couldn’t help themselves. Even Mother Teresa would hate the guy.
Venter proved equally successful in alienating his financial backers. In 2002, Celera fired him and he went into a depression, only to bounce back as head of the privately-funded "Genesis Project," which effectively created life by building a virus from scratch. A team at the State University of New York at Stony Book had accomplished a similar feat shortly before, but their effort had taken three years compared to Venter’s 14 days.
Now science was truly playing God, for better or for worse, with the potential to transform the world or destroy it. It’s the kind of challenge that hypomanics live for.
See the full review on mcmanweb
Columbus, religious dissidents, Alexander Hamilton, Andrew Carnegie, the Hollywood moguls ...
Labels:
Craig Venter,
hypomania,
Hypomanic Edge,
John Gartner,
John McManamy
Thursday, April 15, 2010
Rerun: Treating Marilyn

My most recent blog piece touched on a section of a grand rounds I delivered on meds compliance two years ago at a psychiatric facility in Princeton. That section, "The Problem Clinician," received a decidedly frosty reception from my audience of clinicians. This section, from "The Problem Patient," went over a lot better.
This piece first appeared on my blog in Feb, 2009.
The following is based on the first part of a talk I gave to clinicians on meds compliance as part of a grand rounds at a psychiatric facility in Princeton:
'Marilyn walks into your office," I began. "She reveals her moods have been all over the place. Everything points to bipolar. Okay. How do you treat her?"
Believe it or not, no one raised their hands. I was the one who had to suggest that a mood stabilizer might be a good idea, then I had to make sure we had a consensus. Then I went to the catch, namely how does the most important person in the equation - the patient - feel? After all, even the best med in the world is useless if patients won't take it.
Maybe we need to ask Marilyn a few more questions, I suggested. Consider:
Marilyn is literally larger than life. Over the top is her baseline. It's a legitimate part of her personality. How long do you think she is going to stay on her mood stabilizer if she thinks her personality is getting medicated out of her?
Hypomania is the first thing to come to mind when thinking of Marilyn, but the operative word from the DSM regarding this type of behavior is "uncharacteristic."
"For someone else to act like Marilyn," I said, "that may be hypomanic. For Marilyn to act like Marilyn - that's normal."
In support, I cited Ronald Fieve MD of Columbia University, who coined the term, "the hypomanic advantage."
"Keep in mind," I said, "a lot of us view the world through the eyes of artists and poets and visionaries and mystics. Not to mention through the eyes of highly successful professionals and entrepreneurs. We don't want to be like you."
How can I describe the look of surprise from my audience? Like I had let rip a roof-rattler and they were too polite to laugh - I think that best sums it up. I should have thrown away my prepared talk at that stage. Seriously, I should have said. We don't want to be like you. Why should that surprise you?
Instead I plowed ahead:
"We don't want to fly too close to the sun," I continued. "But don't clip our wings. Obviously Marilyn needs to be reeled in a bit. But how do we proceed? What do we have to go on?"
Believe it or not, there are zero published studies for treating hypomania. Zip, zilch, nada. The only solid evidence base involves the acute phase of full-blown mania, when we're bouncing off walls, 911 cases.
"So," I asked, "are you thinking of giving someone with hypomania an industrial strength dose?"
What else is going on with Marilyn? Personality issues? Quirky behavior? Does the bipolar itself affect her capacity to think rationally?
"You're the rational ones," I said. "We know where you are coming from. But do you know where your patients are coming from?"
I clicked to two slides: Fear/feeling threatened, problems accepting authority, cognitive distortions ...
The list went on and on. "Looking like a lot of your patients?" I asked.
"Here's the point I'm making," I continued. "Not only are you treating the illness. You are treating any behaviors and attitudes that come in the way of treatment. And you're not going to find that out unless you talk to the patient - and listen."
I wasn't through: "Just sending a patient out the door with a prescription - in my opinion - is not treatment."
Back to Marilyn. She's Marilyn. She has enormous gifts and doesn't want her wings clipped. She has various personality issues. And her illness is affecting her judgment.
"We have the advantage of knowing the tragic outcome," I concluded. "Knowing what you know, are you happy just writing her a prescription and sending her out the door?"
Postscript: This first part of my talk - "The Problem Patient" - went fairly well, perhaps because the audience could spin my message in a way that assigned all blame to the patient. There was no way they could do that with the next two sections, "Problem Meds" and "The Problem Clinician," and I got a very different reaction.
More later ...
Labels:
hypomania,
John McManamy,
Marilyn Monroe,
meds,
meds compliance
Wednesday, April 14, 2010
Meds Compliance: The Problem Clinician
Yesterday, I raised the topic of physicians turning a deaf ear to our complaints about meds side effects. The obvious conclusion to draw is that patients will simply stop taking their meds. You don’t need a medical degree to understand that. In fact, it helps if you don’t have one.
Two and a half years ago, a psychiatrist who practices in Princeton, NJ (I used to live just outside Princeton) invited me to deliver a grand rounds to a psychiatric facility there. I was very hesitant. I’m a journalist, I explained. It’s not my place to tell others how to do their jobs.
But I had been doing my own research into meds compliance. Perhaps it would be okay, I suggested, if I were to report on my research from the perspective of a patient. The psychiatrist loved the idea, and we booked a date.
How controversial can meds compliance be, right? I mean, no one is against meds compliance. So I went back over my old research, then did some more, and started connecting the dots. Suddenly, I realized I was in big trouble. Psychiatrists came out looking worse than the patients. A lot worse.
There’s no way I can sugar-coat this, I confided to my friends. They’re going to run me out of town on a rail.
The first part of my talk - “The Problem Patient” - went over reasonably well. But I started sinking fast when I got into “Problem Meds.” Then “The Problem Clinician” went up on my PowerPoint.
Frozen silence. We’re not talking ordinary frozen silence, as in “stony cold” frozen silence. We’re talking zero degrees Kelvin silence, as in utter cessation of all molecular motion frozen silence.
What’s totally weird is they should have been rolling in the aisles. My PowerPoint slide featured a photo of Hugh Laurie from the TV series “House” snapping on a latex glove. “House” is set in Princeton. Surely, my audience would at least chuckle in knowing appreciation.
Silence. Zero degrees Kelvin silence.
Up went a slide of Heidi Klum. “Have you ever noticed how many drug reps look like Heidi Klum?” I asked. Or Russell Crowe?
To paraphrase George Bush, I “misunderestimated” my audience.
Let’s take a look at some of the hard cold facts from my PowerPoint:
Sending patients out the door with just a prescription is not treatment, I reminded them. (They positively hated hearing that.)
Obviously, I went on to say, a clear psychiatric disconnect exists. According to another study by Scott and Pope, clinicians felt their patients quit lithium owing to "missing highs." Patients who quit, on the other hand, cited other reasons.
At the 2006 national NAMI convention, Stephen Goldfinger MD of SUNY told his audience: “Patients will be adherent if the meds do their real job.”
I did my initial research into meds noncompliance about eight years ago when I came across a Kirsch meta-analysis (summarized in a recent piece) that revealed, amongst other things, that only 63 percent of the patients in antidepressant drug trials completed the four to six weeks these trials ran.
Curious, I began checking if these drop-out rates applied across the rest of medicine, such as cancer. So I picked a cancer med at random, Nolvadex (tamoxifen) and read that AstraZeneca had stopped a 1997 study due to 26 percent of patients quitting after one year.
Hmm, I thought. A 74 percent completion rate over one year, significantly higher than the antidepressant completion rate over a mere six weeks. Yet, this was totally unacceptable in the field of cancer. I remember reporting in a Newsletter at the time that a drug company would be touting the exact same completion rate for an antidepressant as a stunning success. Indeed, two weeks later, Lundbeck proved me right by publishing a one-year Lexapro trial that highlighted a mere 26 percent of patients dropping out of the study.
I didn’t bring this up this in my talk. What I did note was that the 26 percent Nolvadex drop-out rate almost exactly corresponded to the 21 percent Zyprexa completion rate.
Psychiatry and oncology clearly have different standards. So, are oncologists telling their patients something different? My guess is they are. I acknowledged to my audience I was speculating, but I managed to get them to sign off on this PowerPoint:
What oncologists may be telling their patients:
It's going to be hell, but there is an excellent chance your cancer will go away.
Then I showed them this PowerPoint:
What I know too many psychiatrists tell their patients:
What are you complaining about? These meds work. Something must be wrong with you. You're much better off than you were before. You need to stay on these drugs the rest of your life.
What I’m guessing the cancer patient may be thinking is this: One year of hell - if that's what it takes to get my old life back, I'm willing to put up with that.
What I know the psychiatric patient is thinking is this: This is the best you can do? You mean I'm going to have to spend the rest of my life - like this?
As Ross Baldessarini MD of Harvard told a 2006 American Psychiatric Association annual meeting: "We need to be a lot more sensitive to minor complaints." Otherwise, "we will drive patients out of treatment."
So maybe psychiatrists need to be working off a bad news/good news script. First the bad news:
Your meds are only part of the equation. You are unique. It may take time to find the right meds and doses that work right for you. Until we dial in your meds just right, you may have to put up with significant side effects. You may also not feel like yourself. You may feel you want to quit altogether.
Now the good news:
We are going to work together on your recovery. As your knowledge and skills improve, I will be in a better position to help you. You will also be in a better position to help yourself. Trust me, there is light at the end of this tunnel.
I wrapped up my talk a few minutes later. The audience, composed entirely of clinicians, showed their appreciation by stampeding for the exits the second my lips stopped moving.
Two and a half years ago, a psychiatrist who practices in Princeton, NJ (I used to live just outside Princeton) invited me to deliver a grand rounds to a psychiatric facility there. I was very hesitant. I’m a journalist, I explained. It’s not my place to tell others how to do their jobs.
But I had been doing my own research into meds compliance. Perhaps it would be okay, I suggested, if I were to report on my research from the perspective of a patient. The psychiatrist loved the idea, and we booked a date.
How controversial can meds compliance be, right? I mean, no one is against meds compliance. So I went back over my old research, then did some more, and started connecting the dots. Suddenly, I realized I was in big trouble. Psychiatrists came out looking worse than the patients. A lot worse.
There’s no way I can sugar-coat this, I confided to my friends. They’re going to run me out of town on a rail.
The first part of my talk - “The Problem Patient” - went over reasonably well. But I started sinking fast when I got into “Problem Meds.” Then “The Problem Clinician” went up on my PowerPoint.
Frozen silence. We’re not talking ordinary frozen silence, as in “stony cold” frozen silence. We’re talking zero degrees Kelvin silence, as in utter cessation of all molecular motion frozen silence.
What’s totally weird is they should have been rolling in the aisles. My PowerPoint slide featured a photo of Hugh Laurie from the TV series “House” snapping on a latex glove. “House” is set in Princeton. Surely, my audience would at least chuckle in knowing appreciation.
Silence. Zero degrees Kelvin silence.
Up went a slide of Heidi Klum. “Have you ever noticed how many drug reps look like Heidi Klum?” I asked. Or Russell Crowe?
To paraphrase George Bush, I “misunderestimated” my audience.
Let’s take a look at some of the hard cold facts from my PowerPoint:
- According to a 2002 study by Scott and Pope, 50% of bipolar patients on mood stabilizers acknowledged some degree of medication nonadherence in the previous 2 years.
- According to a 2007 Swedish study, 25 percent stopped taking their lithium in 45 days. The median time to discontinuation of lithium was 181 days.
- In one of the NIMH-underwritten CATIE schizophrenia trials, no one completed the study.
- In a 2006 long-term Zyprexa trial, nearly 80 percent of the patients on the drug dropped out.
- A 2005 Medscape article reported that only 28% complied with their SSRIs at 6 months.
Sending patients out the door with just a prescription is not treatment, I reminded them. (They positively hated hearing that.)
Obviously, I went on to say, a clear psychiatric disconnect exists. According to another study by Scott and Pope, clinicians felt their patients quit lithium owing to "missing highs." Patients who quit, on the other hand, cited other reasons.
At the 2006 national NAMI convention, Stephen Goldfinger MD of SUNY told his audience: “Patients will be adherent if the meds do their real job.”
I did my initial research into meds noncompliance about eight years ago when I came across a Kirsch meta-analysis (summarized in a recent piece) that revealed, amongst other things, that only 63 percent of the patients in antidepressant drug trials completed the four to six weeks these trials ran.
Curious, I began checking if these drop-out rates applied across the rest of medicine, such as cancer. So I picked a cancer med at random, Nolvadex (tamoxifen) and read that AstraZeneca had stopped a 1997 study due to 26 percent of patients quitting after one year.
Hmm, I thought. A 74 percent completion rate over one year, significantly higher than the antidepressant completion rate over a mere six weeks. Yet, this was totally unacceptable in the field of cancer. I remember reporting in a Newsletter at the time that a drug company would be touting the exact same completion rate for an antidepressant as a stunning success. Indeed, two weeks later, Lundbeck proved me right by publishing a one-year Lexapro trial that highlighted a mere 26 percent of patients dropping out of the study.
I didn’t bring this up this in my talk. What I did note was that the 26 percent Nolvadex drop-out rate almost exactly corresponded to the 21 percent Zyprexa completion rate.
Psychiatry and oncology clearly have different standards. So, are oncologists telling their patients something different? My guess is they are. I acknowledged to my audience I was speculating, but I managed to get them to sign off on this PowerPoint:
What oncologists may be telling their patients:
It's going to be hell, but there is an excellent chance your cancer will go away.
Then I showed them this PowerPoint:
What I know too many psychiatrists tell their patients:
What are you complaining about? These meds work. Something must be wrong with you. You're much better off than you were before. You need to stay on these drugs the rest of your life.
What I’m guessing the cancer patient may be thinking is this: One year of hell - if that's what it takes to get my old life back, I'm willing to put up with that.
What I know the psychiatric patient is thinking is this: This is the best you can do? You mean I'm going to have to spend the rest of my life - like this?
As Ross Baldessarini MD of Harvard told a 2006 American Psychiatric Association annual meeting: "We need to be a lot more sensitive to minor complaints." Otherwise, "we will drive patients out of treatment."
So maybe psychiatrists need to be working off a bad news/good news script. First the bad news:
Your meds are only part of the equation. You are unique. It may take time to find the right meds and doses that work right for you. Until we dial in your meds just right, you may have to put up with significant side effects. You may also not feel like yourself. You may feel you want to quit altogether.
Now the good news:
We are going to work together on your recovery. As your knowledge and skills improve, I will be in a better position to help you. You will also be in a better position to help yourself. Trust me, there is light at the end of this tunnel.
I wrapped up my talk a few minutes later. The audience, composed entirely of clinicians, showed their appreciation by stampeding for the exits the second my lips stopped moving.
Labels:
John McManamy,
meds,
nonadherence,
noncompliance
Tuesday, April 13, 2010
Notice to Readers
For the safety of readers and to preserve the integrity of the comments here, I have tightened the settings for those wishing to make comments. The forums here rely on the good faith of those making comments. It has come to my attention that on several occasions this good faith has been breached. It appears that one individual in particular has assumed several aliases in pursuit of a sick agenda.
There is no perfect system, of course, for keeping the sickos out. Let's see how the new settings work. Sorry for the inconvenience ...
There is no perfect system, of course, for keeping the sickos out. Let's see how the new settings work. Sorry for the inconvenience ...
Three Days to Go for My NAMI Walk
I'm trying really hard to raise money, so please bear with me:
I've been involved in mental health since I was first diagnosed with bipolar 11 years ago, following a lifetime of denial. I used to be a financial journalist, so turning to mental health journalism was my means of coming to terms with my diagnosis. Literally, I wrote myself out of the hole I was in. Here I am, 11 years later, still writing.
Over the years, I have also been in involved in DBSA and NAMI. I was the founding facilitator of a DBSA chapter in Princeton, NJ, and have spoken at national conferences and to local groups. Later this month, I will be flying to Kansas to deliver a keynote address to the Kansas State DBSA Conference. (See side panel for details.)
This Saturday, I will be walking for NAMI.
Over the years, as a journalist, I have had the privilege of hearing the stories of NAMI people from all over the country. I have attended national conferences and I have spoken at state conferences and at local meetings. Since moving to Southern CA from NJ more than three years ago, I have become increasingly involved with NAMI San Diego.
Last year, I was asked to serve on its board, which I regard as a great honor. Even by NAMI standards, NAMI San Diego does incredible work. This includes a very full menu of NAMI signature programs such as In Our Own Voice, Family to Family, and Peer to Peer, not to mention an info line, numerous support groups, educational programs, conferences, partnerships in the community, advocacy, and outreaches to ethnic and cultural minorities.
I could go on and on and on. Suffice to say, over the years, NAMI has been a tremendous comfort, both to myself and my family.
You don't need to be living in the San Diego area to support me on my walk. NAMI San Diego may have a local focus, but a lot of our work here has a national impact, and is used as a model for local NAMIs everywhere. We have a dynamic new Executive Director (who learned the ropes from our legendary recently retired ED), a highly-dedicated (and hugely underpaid) staff, and volunteers who are an inspiration.
So, here's the pitch: We need money. We're a non-profit organization. Our programs are free of charge. We serve many thousands of people a year in San Diego County, but we badly want to serve more. Everybody in fact.
It can be so frustrating at times, from board level, staff level, and volunteer level. So much need in the community, so much that needs to be done, only so much we can do.
All of us here at NAMI San Diego are motivated by doing things. Serving our community. Our only limitation is our limited resources, and you can really help us out.
Please support me in my NAMI walk. Every little bit helps. If you get something out of what I do here on Knowledge is Necessity, this is your way of showing your appreciation. You can make a donation online on my Walk page.
Also, if you live in the area, I cordially invite you to walk with me on Saturday as a member of my walk team, McMan's Silly Walkers. You can join by going to my Team page.
Many thanks.
I've been involved in mental health since I was first diagnosed with bipolar 11 years ago, following a lifetime of denial. I used to be a financial journalist, so turning to mental health journalism was my means of coming to terms with my diagnosis. Literally, I wrote myself out of the hole I was in. Here I am, 11 years later, still writing.
Over the years, I have also been in involved in DBSA and NAMI. I was the founding facilitator of a DBSA chapter in Princeton, NJ, and have spoken at national conferences and to local groups. Later this month, I will be flying to Kansas to deliver a keynote address to the Kansas State DBSA Conference. (See side panel for details.)
This Saturday, I will be walking for NAMI.
Over the years, as a journalist, I have had the privilege of hearing the stories of NAMI people from all over the country. I have attended national conferences and I have spoken at state conferences and at local meetings. Since moving to Southern CA from NJ more than three years ago, I have become increasingly involved with NAMI San Diego.
Last year, I was asked to serve on its board, which I regard as a great honor. Even by NAMI standards, NAMI San Diego does incredible work. This includes a very full menu of NAMI signature programs such as In Our Own Voice, Family to Family, and Peer to Peer, not to mention an info line, numerous support groups, educational programs, conferences, partnerships in the community, advocacy, and outreaches to ethnic and cultural minorities.
I could go on and on and on. Suffice to say, over the years, NAMI has been a tremendous comfort, both to myself and my family.
You don't need to be living in the San Diego area to support me on my walk. NAMI San Diego may have a local focus, but a lot of our work here has a national impact, and is used as a model for local NAMIs everywhere. We have a dynamic new Executive Director (who learned the ropes from our legendary recently retired ED), a highly-dedicated (and hugely underpaid) staff, and volunteers who are an inspiration.
So, here's the pitch: We need money. We're a non-profit organization. Our programs are free of charge. We serve many thousands of people a year in San Diego County, but we badly want to serve more. Everybody in fact.
It can be so frustrating at times, from board level, staff level, and volunteer level. So much need in the community, so much that needs to be done, only so much we can do.
All of us here at NAMI San Diego are motivated by doing things. Serving our community. Our only limitation is our limited resources, and you can really help us out.
Please support me in my NAMI walk. Every little bit helps. If you get something out of what I do here on Knowledge is Necessity, this is your way of showing your appreciation. You can make a donation online on my Walk page.
Also, if you live in the area, I cordially invite you to walk with me on Saturday as a member of my walk team, McMan's Silly Walkers. You can join by going to my Team page.
Many thanks.
Meds Side Effects: Will Doctors Ever Listen?
The headline to an article in yesterday’s NY Times caught my attention:
In Reporting Symptoms, Don’t Patients Know Best?
The article, by Denise Graves, began with a personal account of a drug she was given to treat pain from an injury. A few days later, she woke up with a huge red blister on her tongue and immediately stopped the medication. Her doctor pooh-poohed the blister, writing it off to coincidence.
Later on the drug, Bextra, was taken off the market in the US. Amongst other things, Bextra was linked to the sometimes deadly Stevens-Johnson syndrome, which can cause mouth blisters. Ms Graves was quick to say that maybe the drug did not cause the blisters, but “I never understood why my doctor was so quick to dismiss it.”
Is this resonating with you? I thought so.
Ms Graves cites a recent article by oncologist Ethan Basch in the New England Journal of Medicine that argues that doctors need to pay more attention to patients. According to her account:
Direct reports from patients are rarely used during drug approval or in clinical trials, Dr. Basch says. If patients’ comments are sought at all, they are usually filtered through doctors and nurses, who write their own impressions of what the patients are feeling.
Typically, the clinicians downgrade the severity of the patient’s symptoms, often writing us off as whiners and complainers. Sometimes, “the downgrading may reflect wishful thinking by doctors, who may think that a certain drug will help patients and don’t want to take them off it.”
I’ve written a lot on this kind of stuff, and it’s worth quoting at length from my inaugural blog piece here at Knowledge is Necessity, from late Dec, 2008:
Early in 2008, in preparing for a grand rounds lecture I was to deliver to a psychiatric hospital in Princeton, I came across a 2006 study published in the American Journal of Psychiatry, which is put out by the American Psychiatric Association. The study concerned bipolar patients on Zyprexa, and was designed and written by Eli Lilly, which manufactures the drug.
The article listed Mauricio Tohen MD, DrPH as the lead author of the study. Dr Tohen is virtually unique in psychiatry in that he is affiliated with Harvard and Mass General Hospital AND is employed by Eli Lilly. In addition to Dr Tohen, the article listed eight other authors. Three of the names were instantly recognizable as prominent academic thought leaders.
According to the abstract of the study:
"Compared to placebo, olanzapine delays relapse into subsequent mood episodes in bipolar I disorder patients who responded to open-label acute treatment with olanzapine for a manic or mixed episode."
But the study data, not mentioned in the abstract, told a far different story. In fact, eighty percent of the patients in the study stopped taking their Zyprexa.
When I raised this to my audience of clinicians in my talk, I asked if anyone thought this was deceitful. All hands went up. I would go further, I said. I would say it's immoral.
Zyprexa is an antipsychotic with a high side effects profile, and it's not surprising that four in five bipolar patients choose not to take it, even if they are otherwise doing well on it. As Holly Swartz MD of the University of Pittsburgh told a symposium at the 2006 APA annual meeting: "If a patient doesn’t stay on it, it doesn’t do any good, even if it works.”
My audience, incidentally, entirely clinicians, stampeded to the exits as soon as I finished my talk.
In Reporting Symptoms, Don’t Patients Know Best?
The article, by Denise Graves, began with a personal account of a drug she was given to treat pain from an injury. A few days later, she woke up with a huge red blister on her tongue and immediately stopped the medication. Her doctor pooh-poohed the blister, writing it off to coincidence.
Later on the drug, Bextra, was taken off the market in the US. Amongst other things, Bextra was linked to the sometimes deadly Stevens-Johnson syndrome, which can cause mouth blisters. Ms Graves was quick to say that maybe the drug did not cause the blisters, but “I never understood why my doctor was so quick to dismiss it.”
Is this resonating with you? I thought so.
Ms Graves cites a recent article by oncologist Ethan Basch in the New England Journal of Medicine that argues that doctors need to pay more attention to patients. According to her account:
Direct reports from patients are rarely used during drug approval or in clinical trials, Dr. Basch says. If patients’ comments are sought at all, they are usually filtered through doctors and nurses, who write their own impressions of what the patients are feeling.
Typically, the clinicians downgrade the severity of the patient’s symptoms, often writing us off as whiners and complainers. Sometimes, “the downgrading may reflect wishful thinking by doctors, who may think that a certain drug will help patients and don’t want to take them off it.”
I’ve written a lot on this kind of stuff, and it’s worth quoting at length from my inaugural blog piece here at Knowledge is Necessity, from late Dec, 2008:
Early in 2008, in preparing for a grand rounds lecture I was to deliver to a psychiatric hospital in Princeton, I came across a 2006 study published in the American Journal of Psychiatry, which is put out by the American Psychiatric Association. The study concerned bipolar patients on Zyprexa, and was designed and written by Eli Lilly, which manufactures the drug.
The article listed Mauricio Tohen MD, DrPH as the lead author of the study. Dr Tohen is virtually unique in psychiatry in that he is affiliated with Harvard and Mass General Hospital AND is employed by Eli Lilly. In addition to Dr Tohen, the article listed eight other authors. Three of the names were instantly recognizable as prominent academic thought leaders.
According to the abstract of the study:
"Compared to placebo, olanzapine delays relapse into subsequent mood episodes in bipolar I disorder patients who responded to open-label acute treatment with olanzapine for a manic or mixed episode."
But the study data, not mentioned in the abstract, told a far different story. In fact, eighty percent of the patients in the study stopped taking their Zyprexa.
When I raised this to my audience of clinicians in my talk, I asked if anyone thought this was deceitful. All hands went up. I would go further, I said. I would say it's immoral.
Zyprexa is an antipsychotic with a high side effects profile, and it's not surprising that four in five bipolar patients choose not to take it, even if they are otherwise doing well on it. As Holly Swartz MD of the University of Pittsburgh told a symposium at the 2006 APA annual meeting: "If a patient doesn’t stay on it, it doesn’t do any good, even if it works.”
My audience, incidentally, entirely clinicians, stampeded to the exits as soon as I finished my talk.
Monday, April 12, 2010
This is OUR DSM (Forget About Clinicians)
As you know, I have begun work here on a People’s DSM, with my own version of what depression and bipolar should look like. I suffer from no delusions that clinicians will actually take this seriously. As the title says, this is the People’s DSM, not the Clinician’s DSM.
Let me back up a bit and explain:
The DSM-III of 1980 was intended as a means of clinicians communicating to other clinicians. A nurse on an Indian reservation and a celebrity psychiatrist in an Upper East Side practice talking on the phone, in theory, would each know what the other meant by “depression” or “bipolar” or “schizophrenia.”
In order to accomplish this, however, the DSM was forced to err on the side of simplicity. A lot of the vital nuances were lost, which tended to defeat the purpose. In any case, the DSM was supposed to be the Doctor’s Dictionary. Nothing more.
The totally unexpected overnight success of the DSM-III, however, changed all that. In no time, a mere dictionary morphed into the diagnostic bible, not to mention the clinician’s cheat sheet, with the quickie symptom checklist standing in for sophisticated evaluations and clinical wisdom.
With the DSM becoming the means by which clinicians got paid, total corruption set in, guaranteeing that diagnostic psychiatry would be stuck in a simplistic 1980 mindset forever. From our perspective as patients and loved ones, this meant our own learning would be very narrowly based. The Doctors’ Dictionary sadly turned into The Patients’ Primer. As I explained in an article on mcmanweb last year:
Go to nearly any mental health website (not this one), and you will be treated to descriptions of depression and bipolar based on DSM-IV criteria. Read a book, glance at a brochure, take an online test, talk to your doctor - all DSM all the time.
This is where I got involved. It’s not my place to tell clinicians how to do their jobs. But with our lives on the line, we cannot afford to be as misinformed as they are. That’s what Knowledge is Necessity is all about. On my website, I introduced my DSM Report Cards and The People’s DSM this way:
In February this year, the American Psychiatric Association's DSM-5 Task Force issued its Proposed Revisions to the next edition of the DSM, due out in 2013. The proposals, if enacted, will do very little to change the depression and bipolar diagnoses, but they do provide us with a golden opportunity to rethink issues that we tend to take for granted.
And further on:
Don't worry, no one listens to me. But both exercises are food for thought. Without awareness into our respective conditions, we are at the mercy of clinicians in a hurry. Now, more than ever, knowledge is necessity.
A few hours after I happened to write that, I attended a NAMI "In Our Own Voice" presentation. One of the presenters, let’s call him Adam, mentioned that at different times he had been diagnosed with depression, bipolar, and schizophrenia. Someone in the audience happened to ask why the schizophrenia diagnosis.
We pick up the account on a blog I write for HealthCentral’s BipolarConnect:
Adam explained that when he was depressed he was also experiencing psychotic delusions, which is why his doctor assumed he had schizophrenia. I turned to a friend in disbelief.
This is crazy, I whispered to my friend, a schizophrenia diagnosis on the basis of just one psychotic episode? The doctor has to be an idiot.
Often I get the impression psychiatrists are doctors not smart enough to be proctologists. I went on to say that the current DSM, flawed as it was, should have led Adam’s psychiatrist to a far less extreme diagnostic call. Which leads us to the $64,000 question:
So would an improved DSM have afforded Adam’s doctor greater guidance? No, sad to say. The current DSM was more than adequate, and therein lies the problem: The best diagnostic manual in the world is only as good as the doctor reading it.
As I said to my friend, there are too many idiot doctors out there. Way too many.
So, back to why we are here:
The smart doctors are already practicing psychiatry according to The People’s DSM. All I did was gather their insights, along with yours, and tie them in a bow. So smart clinicians hardly need to change their ways. And the dumb ones who badly need remedial education, well, they’re too dumb to know that.
In short, the People’s DSM is for our benefit only, to get us thinking about issues vital to our well-being. But I would add this qualifier: It is by no means anyone’s final word. This is supposed to be the start of the conversation, not the end of it. The official DSM had the opposite effect.
So, never mind what clinicians think. It’s what WE think that is important. They’re the ones who get paid, but it’s our lives on the line, not theirs. As I keep saying over and over and over, Knowledge is Necessity.
Let me back up a bit and explain:
The DSM-III of 1980 was intended as a means of clinicians communicating to other clinicians. A nurse on an Indian reservation and a celebrity psychiatrist in an Upper East Side practice talking on the phone, in theory, would each know what the other meant by “depression” or “bipolar” or “schizophrenia.”
In order to accomplish this, however, the DSM was forced to err on the side of simplicity. A lot of the vital nuances were lost, which tended to defeat the purpose. In any case, the DSM was supposed to be the Doctor’s Dictionary. Nothing more.
The totally unexpected overnight success of the DSM-III, however, changed all that. In no time, a mere dictionary morphed into the diagnostic bible, not to mention the clinician’s cheat sheet, with the quickie symptom checklist standing in for sophisticated evaluations and clinical wisdom.
With the DSM becoming the means by which clinicians got paid, total corruption set in, guaranteeing that diagnostic psychiatry would be stuck in a simplistic 1980 mindset forever. From our perspective as patients and loved ones, this meant our own learning would be very narrowly based. The Doctors’ Dictionary sadly turned into The Patients’ Primer. As I explained in an article on mcmanweb last year:
Go to nearly any mental health website (not this one), and you will be treated to descriptions of depression and bipolar based on DSM-IV criteria. Read a book, glance at a brochure, take an online test, talk to your doctor - all DSM all the time.
This is where I got involved. It’s not my place to tell clinicians how to do their jobs. But with our lives on the line, we cannot afford to be as misinformed as they are. That’s what Knowledge is Necessity is all about. On my website, I introduced my DSM Report Cards and The People’s DSM this way:
In February this year, the American Psychiatric Association's DSM-5 Task Force issued its Proposed Revisions to the next edition of the DSM, due out in 2013. The proposals, if enacted, will do very little to change the depression and bipolar diagnoses, but they do provide us with a golden opportunity to rethink issues that we tend to take for granted.
And further on:
Don't worry, no one listens to me. But both exercises are food for thought. Without awareness into our respective conditions, we are at the mercy of clinicians in a hurry. Now, more than ever, knowledge is necessity.
A few hours after I happened to write that, I attended a NAMI "In Our Own Voice" presentation. One of the presenters, let’s call him Adam, mentioned that at different times he had been diagnosed with depression, bipolar, and schizophrenia. Someone in the audience happened to ask why the schizophrenia diagnosis.
We pick up the account on a blog I write for HealthCentral’s BipolarConnect:
Adam explained that when he was depressed he was also experiencing psychotic delusions, which is why his doctor assumed he had schizophrenia. I turned to a friend in disbelief.
This is crazy, I whispered to my friend, a schizophrenia diagnosis on the basis of just one psychotic episode? The doctor has to be an idiot.
Often I get the impression psychiatrists are doctors not smart enough to be proctologists. I went on to say that the current DSM, flawed as it was, should have led Adam’s psychiatrist to a far less extreme diagnostic call. Which leads us to the $64,000 question:
So would an improved DSM have afforded Adam’s doctor greater guidance? No, sad to say. The current DSM was more than adequate, and therein lies the problem: The best diagnostic manual in the world is only as good as the doctor reading it.
As I said to my friend, there are too many idiot doctors out there. Way too many.
So, back to why we are here:
The smart doctors are already practicing psychiatry according to The People’s DSM. All I did was gather their insights, along with yours, and tie them in a bow. So smart clinicians hardly need to change their ways. And the dumb ones who badly need remedial education, well, they’re too dumb to know that.
In short, the People’s DSM is for our benefit only, to get us thinking about issues vital to our well-being. But I would add this qualifier: It is by no means anyone’s final word. This is supposed to be the start of the conversation, not the end of it. The official DSM had the opposite effect.
So, never mind what clinicians think. It’s what WE think that is important. They’re the ones who get paid, but it’s our lives on the line, not theirs. As I keep saying over and over and over, Knowledge is Necessity.
Sunday, April 11, 2010
Rerun: Trick Question - Vincent Van Gogh

This from Feb 2009 ...
Between Feb 1888 and May 1889, Vincent Van Gogh produced an incredible 187 paintings. How many did he produce from Aug 1890 to Sept 1891?
Answer: Zero. On a brilliant day in July 1890, Van Gogh aimed a pistol at his chest and fired. He died two days later. He was 37. The paintings would stop. There would be no more Van Goghs. No more Sunflowers, Irises, or Starry Nights.
Undoubtedly, Van Gogh's madness stoked his creativity. But it also stopped it dead in its tracks.
His last words were: "The sadness will live forever."
From mcmanweb: Vincent and Me
In May of 1889 he entered the asylum at Saint Remy de Provence. "As for me, my health is good," he wrote his brother Theo, "and as for my brain, that will be, let us hope, a matter of time and patience."
***
What got me started on this quick blog was Therese Borchard's excellent video blog from earlier today:
On Creativity and Mood Disorders
Friday, April 9, 2010
Thursday, April 8, 2010
My DSM-5 Commentaries: In Search of Elephant, Willing to Settle for Hippopotamus
A quick update. In early February, the American Psychiatric Association's DSM-5 Task Force issued its Proposed Revisions to the next DSM, due out in 2013. Soon after, on this blog, I began writing some review pieces, which developed into Report Cards highly critical of the draft DSM-5's treatment of depression and bipolar.
This in turn led to my "People's DSM" with its own Alternative Depression Diagnosis and Alternative Bipolar Diagnosis.
The point of both exercises was to get us thinking about issues we tend to take for granted, but which have a profound impact on our well-being.
Needless to say, these are issues with a long shelf life. A blog, on the other hand, tends to be very ephemeral, based on what people do with yesterday's newspaper - namely, you wrap fish in it.
Consequently, I went over my DSM-5 pieces, worked them into article shape, then assembled them in a manner that allowed for coherent reading and review. Last night, I uploaded the effort to my website, McMan's Depression and Bipolar Web. My website is based on the concept of a reference library - information is stored there, in easy-to-find places, there when you need it.
Clicking on a link in the navigation bar on all 200 or so pages of the site takes you to a band new DSM-5 section with eight articles.
The Draft DSM-5: Rip it Up and Start Over is based on two or three blog pieces that first appeared here. The article gives historical background into mood disorders and how Freud and Kraepelin and their followers set the tone for DSMs I through IV. The article also details what went wrong with the draft DSM-5.
My Report Cards set out the issues the various DSM-5 working groups needed to consider, but failed to do, such as clarifying the relationship between unipolar depression and bipolar, rethinking bipolar as a cycling illness, doing something about the schizoaffective diagnosis, making symptom criteria gender-neutral, and so on. Thus:
Grading Depression
Grading Bipolar - Part I
Grading Bipolar - Part II
Think of my Report Cards as the background commentary to my People's DSM, in which I offer an alternative reality to the one imposed on us by the official DSM. Thus:
My Alternative Depression Diagnosis - Part I
My Alternative Depression Diagnosis - Part II
My Alternative Bipolar (Cycling) Diagnosis - Part I
My Alternative Bipolar (Cycling) Diagnosis - Part II
I make no claims to having a better view of reality. Reality is far too vast and elusive to stand still for our own convenience. Basically, we're the six blind men in search of the concept of "elephant." We're never going to achieve "elephant," but perhaps if we keep poking around long enough in the dark, we may come up with something that reasonably approximates elephant, such as "hippopotamus."
Anyway, I encourage you to visit my website, have a new look at points of view you first read about here, leave your comments, and come back here for who knows what we'll stumble upon next.
This in turn led to my "People's DSM" with its own Alternative Depression Diagnosis and Alternative Bipolar Diagnosis.
The point of both exercises was to get us thinking about issues we tend to take for granted, but which have a profound impact on our well-being.
Needless to say, these are issues with a long shelf life. A blog, on the other hand, tends to be very ephemeral, based on what people do with yesterday's newspaper - namely, you wrap fish in it.
Consequently, I went over my DSM-5 pieces, worked them into article shape, then assembled them in a manner that allowed for coherent reading and review. Last night, I uploaded the effort to my website, McMan's Depression and Bipolar Web. My website is based on the concept of a reference library - information is stored there, in easy-to-find places, there when you need it.
Clicking on a link in the navigation bar on all 200 or so pages of the site takes you to a band new DSM-5 section with eight articles.
The Draft DSM-5: Rip it Up and Start Over is based on two or three blog pieces that first appeared here. The article gives historical background into mood disorders and how Freud and Kraepelin and their followers set the tone for DSMs I through IV. The article also details what went wrong with the draft DSM-5.
My Report Cards set out the issues the various DSM-5 working groups needed to consider, but failed to do, such as clarifying the relationship between unipolar depression and bipolar, rethinking bipolar as a cycling illness, doing something about the schizoaffective diagnosis, making symptom criteria gender-neutral, and so on. Thus:
Grading Depression
Grading Bipolar - Part I
Grading Bipolar - Part II
Think of my Report Cards as the background commentary to my People's DSM, in which I offer an alternative reality to the one imposed on us by the official DSM. Thus:
My Alternative Depression Diagnosis - Part I
My Alternative Depression Diagnosis - Part II
My Alternative Bipolar (Cycling) Diagnosis - Part I
My Alternative Bipolar (Cycling) Diagnosis - Part II
I make no claims to having a better view of reality. Reality is far too vast and elusive to stand still for our own convenience. Basically, we're the six blind men in search of the concept of "elephant." We're never going to achieve "elephant," but perhaps if we keep poking around long enough in the dark, we may come up with something that reasonably approximates elephant, such as "hippopotamus."
Anyway, I encourage you to visit my website, have a new look at points of view you first read about here, leave your comments, and come back here for who knows what we'll stumble upon next.
Wednesday, April 7, 2010
The Asshole Effect

I came across this piece from last July very much by accident, having forgotten I'd written it. So much for lasting impressions. Anyway, it's a perfect fit to my other recent pieces on the topic of assholes. Enjoy ...
My most recent blog piece focused on the negativity people in my position attract. Call it the asshole effect. We’ve all had to deal with it. Knock on any door, these idiots are everywhere - people who hate Helen Keller, find fault in a sunset, and think cat food is fillet of cat, which they gleefully describe as tasting like chicken.
Their values are not our values. Hate thy neighbor, the Radioactive Plutonium Rule, It is better to receive than to give ... Whereas we struggle mightily trying to become better people, they cruise through life doing what comes naturally. Ironically - they are the miserable ones.
But it tends to be our friends and loved ones who hurt us most. From assholes, we know what to expect. From those close to us, the unexpected amounts to the unkindest cut of all.
Funny thing, a hundred individuals can heap praise on us - yet we vividly recall the one negative comment. Your dear friend throws himself in front of a car to save your life - you’re furious because three days ago he forgot your birthday.
What is it about us?
Today, by pure chance, I came across a blog piece on Psychology Today by self-described generalist, Jeremy Sherman PhD.
“We are all thin skinned,” he writes. “No one likes hearing anything that feels discouraging or critical. We don’t welcome news that feels like a setback, a loss of status, a loss of gained momentum. We find unpleasant anything that seems to say, ‘you missed a spot’ ..."
No surprise here. Here’s the eye-opener. Citing Jonah Lehrer, author of “How We Decide,” Dr Sherman documents how “loss aversion” contributes to irrational behavior: “Loss aversion explains why sustainable partnerships are ones in which positive encounters outweigh negative ones, five to one.”
Wait! Hold on! It takes FIVE positive encounters to offset ONE negative one? Apparently so. Not only that, any interaction only slightly ambiguous tends to get moved into the negative column. No wonder we’re so miserable.
I’m assuming Dr Sherman is talking about normal people. What about poor shmucks like us? We depressive types can’t seem to help it. We tend to give no weight to positive events and assign disproportionate value to the negative ones. Not only that, we tend to interpret neutral or only slightly encouraging events as negative.
So what does it take for us to balance the scales? A hundred positive events? No wonder we’re so miserable. Fortunately (I use the term loosely) I have bipolar. I have a tendency to over-react to good news. For instance, today I found out that a meteor did not fall on my head, and I’m ecstatic about that.
So what is going on here? Can we point to a system malfunction in the brain? Last month, at the Eighth International Conference on Bipolar Disorder in Pittsburgh, I came across a recent fMRI study that pinpointed a certain location in the brain that appears to be responsible for bipolars over-reacting to both reward and disappointment.
It’s as if we can’t turn our brains off.
The brain studies are coming in thick and fast. A lot of stuff is going on beneath the skull. Naturally, it’s easy - with our brains, especially - to interpret these findings as proof that we’re hard-wired for failure. Not necessarily. The brain is a work-in-progress and we can influence its development.
Granted, sometimes - often - it seems like we’re pushing a rock uphill. It helps if we have four muscular individuals in our scrum, shoulders to the boulder. But all it takes is one asshole, perched smugly above, with an extended pinky jabbing at our rock.
Screw you, asshole! This rock is running you over!
Tuesday, April 6, 2010
The Asshole Diagnosis - And the Asshole Paradox

Finally, it's out in the open. On April Fools Day, I reran my two previous "Asshole" blog posts. The first one, Psychiatry Comes Up with New Diagnosis of Asshole, reported that the new diagnosis offers neither symptoms nor a description, but that "you know one when you see one." The piece noted that bipolars have complained bitterly since the dawn of time over being confused with assholes.
So have sociopaths. As Charles Manson from his prison cell observed: "For years, assholes have been giving us sociopaths a bad name."
So who are we talking about, really? In a comment to my first piece, Registered Psych Nurse wrote:
You do know that this unofficial diagnosis has been used by staff in cutting edge mental health units for decades already. It is an optional term for antisocial or borderline personality disordered individuals, as part of staff dark humor and calling spades spades really. Not all a-holes have aspd or borderline PD it is true, but the vast majority with these disorders do qualify as a-holes.
She goes on to say:
Certainly there is an issue with borderline PDs being misdiagnosed as bipolar disorder - hence the borderline a-holes are bringing an undeserved bad name on real bipolars. Blame the pharmaceutical companies, they encourage Drs to shunt the borderlines under the bipolar classification because this way it's allowable to prescribe more drugs to them. Not ones that they need but oh well. I guess the pharmaceutical pushers may be a-holes too.
Thank you, Registered Psych Nurse for finally putting the issue on the table. Screw being polite. Screw being PC. Let's embrace Registered Psych Nurse for calling it as it truly is, namely: Borderline is the true Asshole diagnosis.
Hear me out:
I got motivated to investigate this in depth about five years ago when I was on the board of a state DBSA back east. It turned out our board was way over-represented by assholes. It also turned out that since these individuals predictably lacked the capacity to hold down a job or a relationship they had all the time in the world to drive people like me crazy.
Since I had the bad luck to be temporarily serving as board president, I had to be nice to these assholes. I put up with their manipulations and lying and backstabbing, their petty complaints, their hissy fits, their meltdowns, their gossip, their personal abuse, their poison pen emails ... It goes on and on. And on and on.
This can't possibly be bipolar behavior, I reasoned. This has to be something else. Then a light went off.
For years, psychiatry has been treating all emotionally volatile individuals as if they had bipolar. That is beginning to change, but we have a long way to go. Last year, in recognition of May as borderline personality disorder month, I did a four-part series on borderline, which essentially boils down to this:
When those with mood disorders respond to treatment they go back to being nice people again (or at least only minor dickheads). Those with borderline remain assholes.
Now here's the tragedy, as I see it: A true asshole is totally unaware of his or her condition. They act as if the whole rest of the world is at fault. They don't want to change. This is very much the opposite of someone seeking out psychiatric or therapeutic services. They know something is wrong. They want to change.
But they're frustrated in their mission if they're given a bipolar diagnosis. They seek help willing to take responsibility, and instead are sent out the door with a prescription and a sense of absolution.
This is an entirely different proposition from those who have received a correct diagnosis, who have accepted their diagnosis, and are willing to put in the work. Call it the asshole paradox: Simply by owning up to the fact of being an asshole, you are well on your way to becoming an ex-asshole.
(Think of the individual in the picture caught on the horns of a dilemma.)
So, yes, let's call a spade a spade: Borderline is the asshole diagnosis. But let's also recognize the asshole paradox.
Let's also recognize the exceptional bravery of those who are willing to own up to their diagnosis in the company of others. It would be so much easier for them to hide behind a bipolar diagnosis. Trust me, the stigma of having bipolar is nothing compared to what those with borderline have to put up with. A little enlightenment from the rest of us is long overdue.
As for true assholes, screw 'em.
Further reading from Knowledge is Necessity:
May is Borderline Personality Disorder Awareness Month
Borderline Personality Disorder - Searching for Respect
Piecing Together the Borderline Puzzle
The Borderline Personality Disorder Matzoh Ball
Monday, April 5, 2010
The People’s DSM: My Alternative Bipolar (Cycling) Diagnosis - Part IV
Okay, time for the boring stuff. In my alternative depression diagnosis, I sensibly restored complexity to an inexcusably oversimplified illness. Bipolar demands an opposite approach. Strip the illness to its essentials and we are talking about a cycle involving down and up, where up simply has to be higher than down.
Concentrate on the fact that we are dealing with a cycling phenomenon, and sensible treatment and illness-management is more likely to follow.
Nevertheless, it’s prudent to add shading and texture. Thus, Cycling I, II, and III, plus cyclothymia - plus (as specifiers) allowances for mixed phases (essentially out-of-phase cycles), plus (more specifiers) the reality of various psychosis complications. These were all dealt with in Part I, Part II, and Part III to my Alternative Bipolar Diagnosis.
In Part IV, I’m going with yet more specifiers (and modifiers), but in keeping with a rough draft (and to keep from boring you to tears) I’m just going with the bare bones, short and sweet.
Cycling Specifiers
Timing: Short phases or long? Undetermined? Short intervals of remission or long? Undetermined?
Rapid cycling, ultra-rapid cycling, and ultradian cycling would be included here. Important point: Here’s why “bipolar” is an erroneous name for what should more accurately be called cycling illness. Bipolar places priority on the episode over the cycle. So, technically, under the current DSM, someone who cycles up and down and back again in the course of a week is not in an episode (as the minimum is a week for mania) long enough to qualify for a bipolar diagnosis.
WTF? True, we don’t want to diagnose someone with a mental illness who is feeling out of sorts for just a day or two. But indisputable evidence of a cycle clearly trumps minor quibbles over length of episode (or, more accurately, cycle phase). Looking at it another way, if you’re cycling that fast you’re in a special kind of episode (phase) that is clearly playing havoc with your life.
Reducing mania and hypomania to a two-day minimum obviates a lot of these concerns. (Note to self: include an exception to the depression and mania and hypomania time minimums where there is clear evidence of ultra-rapid or ultradian cycling.)
Emphasis: Mostly depressed? Mostly manic? Mostly hypomanic? Mostly mixed? Undetermined?
People with “bipolar” tend to be depressed three times longer than they are manic or hypomanic, with residual symptoms persisting even longer. Individuals with bipolar II stay depressed for even longer. If that’s the case, this needs to be spelled out. Likewise if an individual is manic/hypomanic or in various mixed phases most of the time. It makes no sense to give individuals a vague diagnosis with no indication of what their particular version of crazy looks like.
Most recent phase: Depression? Up? Mixed?
This is straight out of the current DSM playbook.
Severity:
Particular phases of the cycle may be relatively benign, but the demands of adjusting to these phase changes may be too much to handle. Loving one day, hostile the next? Not a way to stay in a relationship or hold down a job.
Sleep Specifiers
Our next specifier would bring sleep into consideration, as disruptions to the sleep cycle and the mood cycle are strongly linked. Indeed, one can make a strong case that the mood disorder is the downstream effect of the sleep disorder. Another way of looking at it: Addressing the sleep issues resolves a lot of the mood issues.
We can make this as complicated as we like, but let’s opt for simplicity:
Sufficient consolidated and undisturbed night sleep: Yes? No?
Sufficient daytime wakefulness to meet work and personal obligations and self-enjoyment? Yes? No?
Sleep/wake phase delay/advancement: Yes? No?
Dimensional Specifiers
These cut across diagnostic categories and would be the same as for the Alternative Depression Diagnosis, only linked (if possible) to each phase. Otherwise, to the diagnosis as a whole. Thus:
... with anxiety.
... with personality complications.
(Note to self: the depression phase would also include suicidality and other specifiers from the Alternative Depression diagnosis.)
Severity Specifier
We mentioned severity in relation to the cycle. Normally, each phase would require its own severity specifiers, as well, but mission already accomplished for the up phases in the form of Cycling I, II, and III. For the depression phase, we copy and paste from the Alternative Depression diagnosis.)
Modifiers
I distinguish “modifier” from “specifier” by virtue of how gender, age, and cultural identity may affect the course and presentation of the illness. Depressed women, for instance, are more likely to act in accord with current DSM criteria (such as “appears tearful”) while men who express their psychic pain as anger are likely not to get diagnosed. I’m not sure how this plays out for mania, but let’s make room for discussion.
Child and Adolescent onset deserves special consideration. The current DSM lacks an early-onset specifier for bipolar, which can be interpreted to mean that the illness manifests similarly in kids and adults. Except for the fact that this is not the case. Kids tend to cycle far more rapidly, often in the course of a day with a clear relation to sleep/wake cycle disturbances. Moreover, kids tend to experience mixed phases that are expressed as severe rages.
Thus, if we keep the criteria for cycling and mixed states (not to mention sleep) unrealistically narrow (as under the current DSM), both adults and kids are left out in the cold. The simple solution is to widen these criteria (as we have already done), and include the early onset modifier. This would keep the diagnosis consistent across the life-span, while allowing scope for differences in presentation.
Note the diagnosis remains sufficiently narrow to distinguish cycling from other forms of kid behavior. Nevertheless, there is considerable room for discussion in dealing with kids’ issues, so feel free to fire away.
Conclusion
This wraps up my Alternative Bipolar (Cycling) Diagnosis for now, but we’re by no means finished. Please feel free to join the conversation. Comments below ...
Concentrate on the fact that we are dealing with a cycling phenomenon, and sensible treatment and illness-management is more likely to follow.
Nevertheless, it’s prudent to add shading and texture. Thus, Cycling I, II, and III, plus cyclothymia - plus (as specifiers) allowances for mixed phases (essentially out-of-phase cycles), plus (more specifiers) the reality of various psychosis complications. These were all dealt with in Part I, Part II, and Part III to my Alternative Bipolar Diagnosis.
In Part IV, I’m going with yet more specifiers (and modifiers), but in keeping with a rough draft (and to keep from boring you to tears) I’m just going with the bare bones, short and sweet.
Cycling Specifiers
Timing: Short phases or long? Undetermined? Short intervals of remission or long? Undetermined?
Rapid cycling, ultra-rapid cycling, and ultradian cycling would be included here. Important point: Here’s why “bipolar” is an erroneous name for what should more accurately be called cycling illness. Bipolar places priority on the episode over the cycle. So, technically, under the current DSM, someone who cycles up and down and back again in the course of a week is not in an episode (as the minimum is a week for mania) long enough to qualify for a bipolar diagnosis.
WTF? True, we don’t want to diagnose someone with a mental illness who is feeling out of sorts for just a day or two. But indisputable evidence of a cycle clearly trumps minor quibbles over length of episode (or, more accurately, cycle phase). Looking at it another way, if you’re cycling that fast you’re in a special kind of episode (phase) that is clearly playing havoc with your life.
Reducing mania and hypomania to a two-day minimum obviates a lot of these concerns. (Note to self: include an exception to the depression and mania and hypomania time minimums where there is clear evidence of ultra-rapid or ultradian cycling.)
Emphasis: Mostly depressed? Mostly manic? Mostly hypomanic? Mostly mixed? Undetermined?
People with “bipolar” tend to be depressed three times longer than they are manic or hypomanic, with residual symptoms persisting even longer. Individuals with bipolar II stay depressed for even longer. If that’s the case, this needs to be spelled out. Likewise if an individual is manic/hypomanic or in various mixed phases most of the time. It makes no sense to give individuals a vague diagnosis with no indication of what their particular version of crazy looks like.
Most recent phase: Depression? Up? Mixed?
This is straight out of the current DSM playbook.
Severity:
Particular phases of the cycle may be relatively benign, but the demands of adjusting to these phase changes may be too much to handle. Loving one day, hostile the next? Not a way to stay in a relationship or hold down a job.
Sleep Specifiers
Our next specifier would bring sleep into consideration, as disruptions to the sleep cycle and the mood cycle are strongly linked. Indeed, one can make a strong case that the mood disorder is the downstream effect of the sleep disorder. Another way of looking at it: Addressing the sleep issues resolves a lot of the mood issues.
We can make this as complicated as we like, but let’s opt for simplicity:
Sufficient consolidated and undisturbed night sleep: Yes? No?
Sufficient daytime wakefulness to meet work and personal obligations and self-enjoyment? Yes? No?
Sleep/wake phase delay/advancement: Yes? No?
Dimensional Specifiers
These cut across diagnostic categories and would be the same as for the Alternative Depression Diagnosis, only linked (if possible) to each phase. Otherwise, to the diagnosis as a whole. Thus:
... with anxiety.
... with personality complications.
(Note to self: the depression phase would also include suicidality and other specifiers from the Alternative Depression diagnosis.)
Severity Specifier
We mentioned severity in relation to the cycle. Normally, each phase would require its own severity specifiers, as well, but mission already accomplished for the up phases in the form of Cycling I, II, and III. For the depression phase, we copy and paste from the Alternative Depression diagnosis.)
Modifiers
I distinguish “modifier” from “specifier” by virtue of how gender, age, and cultural identity may affect the course and presentation of the illness. Depressed women, for instance, are more likely to act in accord with current DSM criteria (such as “appears tearful”) while men who express their psychic pain as anger are likely not to get diagnosed. I’m not sure how this plays out for mania, but let’s make room for discussion.
Child and Adolescent onset deserves special consideration. The current DSM lacks an early-onset specifier for bipolar, which can be interpreted to mean that the illness manifests similarly in kids and adults. Except for the fact that this is not the case. Kids tend to cycle far more rapidly, often in the course of a day with a clear relation to sleep/wake cycle disturbances. Moreover, kids tend to experience mixed phases that are expressed as severe rages.
Thus, if we keep the criteria for cycling and mixed states (not to mention sleep) unrealistically narrow (as under the current DSM), both adults and kids are left out in the cold. The simple solution is to widen these criteria (as we have already done), and include the early onset modifier. This would keep the diagnosis consistent across the life-span, while allowing scope for differences in presentation.
Note the diagnosis remains sufficiently narrow to distinguish cycling from other forms of kid behavior. Nevertheless, there is considerable room for discussion in dealing with kids’ issues, so feel free to fire away.
Conclusion
This wraps up my Alternative Bipolar (Cycling) Diagnosis for now, but we’re by no means finished. Please feel free to join the conversation. Comments below ...
Subscribe to:
Posts (Atom)